Enteral nutrition (EN) is provided for patients that have a functioning lower gastrointestinal (GI) tract but are unable to orally ingest nutrients and medication and are at risk for malnutrition.[1] Feeding tubes (Tubes) provide these patients essential nutrition, life-sustaining medications and hydration. Numerous conditions may necessitate long-term EN, including GI dysfunction, cancer, cystic fibrosis, neurological disorders, burn patients, congenital heart disease, Alzheimer’s disease, Parkinson’s disease, and congenital metabolic abnormalities.[1,2] Maintaining Tube patency is critical for many, as EN interruptions are often associated with poor clinical outcomes. Tube clogging (see Figure 1) is the most frequently reported mechanical complication associated with feeding tubes, with reported clogging rates ranging from 9-35%.[3-5] A recent survey of Oley Foundation members (180+ patients with feeding tubes and/or caretakers) indicated that up to 81% of non-acute Tubes become clogged, with 39.4% requiring a tube replacement due to clogs.[6] Clogs result in the interruption of patient’s nutrition and medication regimens, representing a burden to both caregivers and patients.



Figure 1: Images of actual clogged feeding tubes submitted by three (3) different hospitals to Actuated Medical, Inc.
Common approaches to maintain Tube patency include regular flushing with water, carbonated sodas, and enzymatic solutions immediately after administering nutrition or medication. Some healthcare facilities add procedures for adequately crushing medications to prevent clogs. Current methods for unclogging Tubes are time-consuming and unreliable, often ending in patients having to undergo Tube replacements. Tube replacements are associated with their own set of risks, including the need for patient transport to the hospital, transfer to interventional radiology (IR) for radiological guidance or Tube placement confirmation following placement, exposing patients to radiation exposure, or surgical interventions which can expose patients to anesthesia.[7-10] Moreover, Tube misplacements into the bronchial tree reportedly occur in 2.4-3.2% of all nasogastric (NG) tube insertions,[11] a serious complication which, if unidentified, results in pneumonitis, pneumonia, and/or pneumothorax.[11]
Actuated Medical, Inc. (AMI) aimed to directly compare the prophylactic use of the TubeClear system, an actuated mechanical clearing device, to standard practice water flushes at reducing inner wall Tube material buildup, as a means of reducing subsequent material adherence and Tube clogging in vitro. Establishing protocols that could minimize clog formation would be invaluable for maintaining Tube patency and allowing for nutrition and medication regimens to remain uninterrupted.
Methods
Nasogastric (NG) tubes (N=22, 10Fr, 42”) were partially clogged with feeding formula and fiber supplement mixture. Mixture was introduced and blown through with air, coating the Tube inner walls and dried (55°C for 3 hrs.). Tubes were placed in a 3D gastrointestinal model and pump fed (21 mL/hr.) until Tube length was entirely filled with formula (see Figure 2). Half of the Tubes (n=11) were subsequently flushed with 30 mL of water, as directed by clinical practice following feeding formula introduction. The other half of tubes (n=11) underwent a 30 mL water flush in coordination with use of the TubeClear system according to the manufacturer’s instructions. Following clearing procedures, Tubes were dried (55°C for 3 hrs.) to remove moisture introduced by water flushes. Tubes were weighed before and after mixture introduction to quantify the mass within Tubes. As such, the final recorded masses within Tubes were a combination of the initial introduced mixture and added pump fed formula. These mean values did not differ by clearing treatment (0.248 vs 0.250 g, Water vs TubeClear, unpaired T-test, p=0.76) prior to drying. Tubes were weighed following clearing and drying and percent mass increase or decrease from initial mixture mass were calculated (see Figure 3).
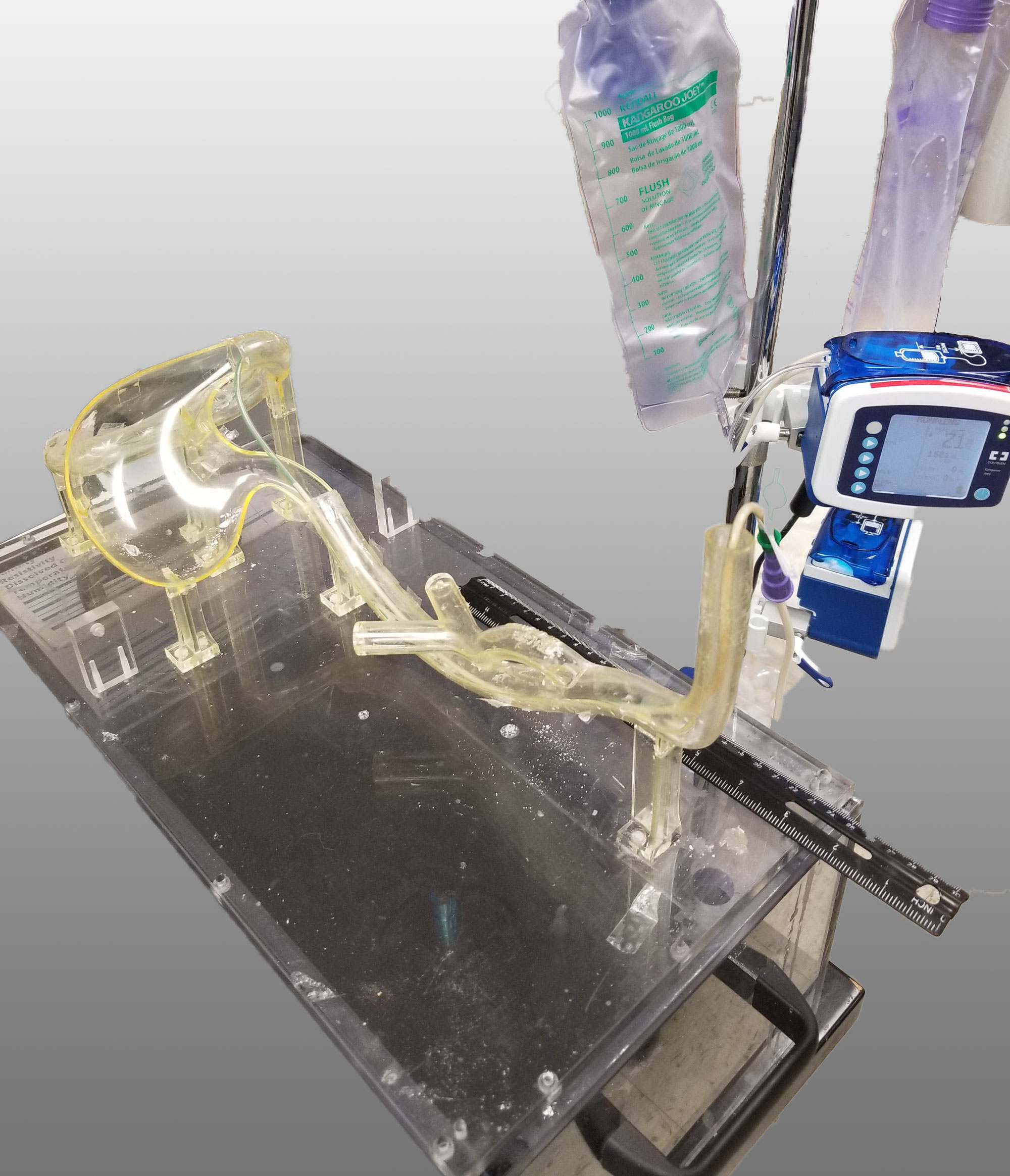
Figure 2: Tube in GI model being pumped with formula.
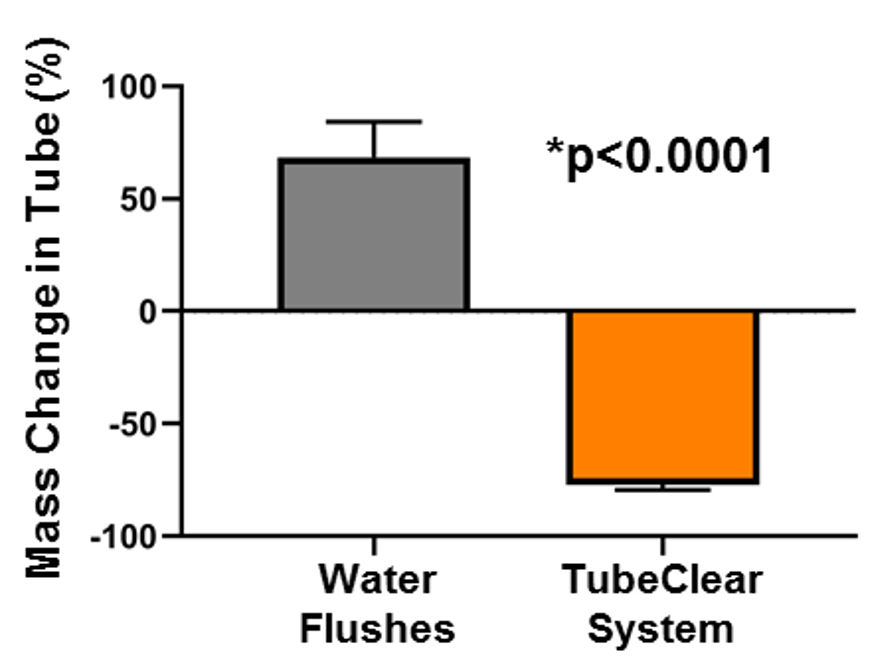
Figure 3: Percent change in mass of NG tubes flushed with with either water alone (Gray Bar) or in conjunction of the TubeClear system (Orange Bar) to remove buildup residue within Tube inner walls. N=22, 11/treatment; Unpaired T-test for significance, Bars= standard error of the mean. *p <0.0001.
Results
The TubeClear system in conjunction with water flushes removed 77.1±2.4% of mass while Water flushing alone added 68.5±15.8% (see Figure 3, unpaired T-test p<0.0001).[12] As added water was removed by post-clearing drying, the added mass, in Water group, was likely formula sticking to the pre-existing Tube material buildup. Images of the partially clogged feeding tubes treated with water or combined with the TubeClear system demonstrated visual differences (see Figure 4), confirmed with mass measurements.
- All Tubes cleared by TubeClear decreased in mass, while nearly all the Tubes flushed with water alone, increased in mass.
- The TubeClear system was 145.6% more effective than water alone at removing buildup.
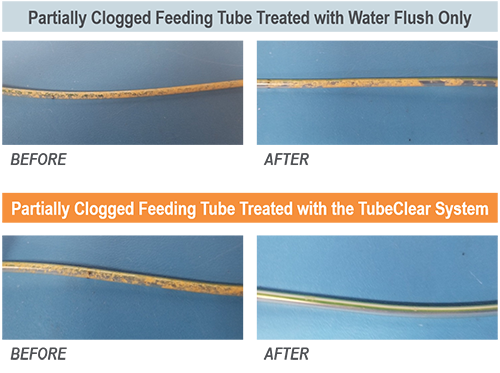
Figure 4: Representative examples of partially clogged feeding tubes treated with water alone (top) or in conjunction with the TubeClear system (Bottom) to remove buildup residue within Tube inner walls.
Conclusions
This work demonstrates that compared to water flushes alone, proactive use of the TubeClear system prior to Tube occlusions can minimize added material buildup from adhering to Tube inner walls, maintaining full Tube diameter and reducing the risk of future clogging, enabling uninterrupted and optimal EN delivery.
References:
- Ireton-Jones C, DeLegge M. Handbook of Home Nutrition Support. Sudburry, MA: Jones and Bartlett; 2007.
- Pederson A. Enteral Feeding (Tube Feeding). Gaining and Growing: Assuring Nutritional Care of Preterm Infants. http://depts.washington.edu/growing/Nourish/Tubes.htm. Accessed2000.
- Marcuard SP, Stegall KS. Unclogging feeding tubes with pancreatic enzyme. JPEN J Parenter Enteral Nutr. 1990;14(2):198-200.
- Bourgault AM, Heyland DK, Drover JW, Keefe L, Newman P, Day AG. Prophylactic pancreatic enzymes to reduce feeding tube occlusions. Nutr Clin Pract. 2003;18(5):398-401.
- Shiram K, Jayanth, V., Lakshmi, R., George, V. Prophylactic Locking of Enteral Feeding Tubes With Pancreatic Enzymes. Journal of Parenteral and Enteral Nutrition. 2012;21(6):353-356.
- Oley Foundation Member Survey: Enteral Feeding Tube Clogging and Resolution. In: Actuated Medical, Inc.; 2015.
- Mathus-Vliegen L, Koning H. Percutaneous endoscopic gastrostomy and gastrojejunostomy: a critical reappraisal of patient selection, tube function and the feasibility of nutritional support during extended follow-up. Gastrointest Endosc. 1999;50(6):746-754.
- Sy K, Dipchand A, Atenafu E, et al. Safety and effectiveness of radiologic percutaneous gastrostomy and gastro jejunostomy in children with cardiac disease. AJR Am J Roentgenol. 2008;191(4):1169-1174.
- Towbin R, Ball WJ, Bissett Gr. Percutaneous gastrostomy and percutaneous gastrojejunostomy in children: antegrade approach. Radiology. 1988;168(2):473-476.
- Smith R-M, Myers S. 2 devices that unclog feeding tubes. RNWeb. http://rn.modernmedicine.com/rnweb/article/articleDetail.jsp?id=142656#intro. Published 2005. Accessed March 9, 2010.
- Stayner JL, Bhatnagar A, McGinn AN, Fang JC. Feeding tube placement: errors and complications. Nutr Clin Pract. 2012;27(6):738-748.
- Actuated Medical Inc. TubeClear Prophylactic Test Report: 1100791569, Rev002. 2019.